Chronic Pelvic Pain
Chronic pelvic pain means pain in the lower part of the stomach or in the pelvis that lasts more than 6 months. This pain can affect both women and men, and it happens to millions of people around the world.
- For Patients
- For Physicians
What Is Chronic Pelvic Pain?
Chronic pelvic pain means pain in the lower part of the stomach or in the pelvis that lasts more than 6 months. This pain can affect both women and men, and it happens to millions of people around the world.1 SAFIRE is working to help people with this kind of pain by focusing on three main causes:
- Iliac vein compression
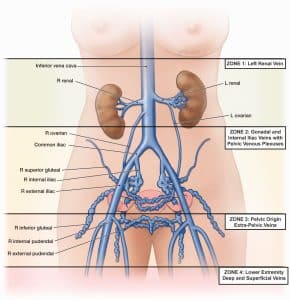
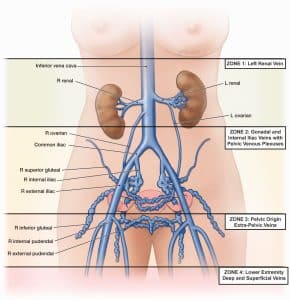
- Pelvic varicose veins
- Gonadal vein reflux
These are called pelvic venous disorders (or PeVD for short).
- Iliac Vein Compression
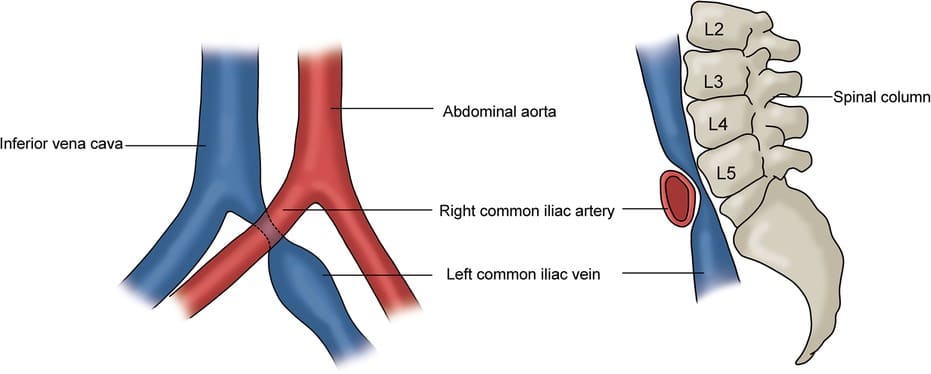
This happens when a big artery (blood vessel that carries blood from your heart to your legs) pushes down on a nearby vein (which carries blood back to your heart).2 This squeeze can block blood from moving normally, causing it to build up in your pelvis. When that happens, veins stretch and pain sensors in the vein wall can cause pain symptoms. The enlarged veins may also affect nerves in the area. The pressure from the built up blood can cause long-lasting pain.3
- Pelvic Varicose Veins
Just like people can get varicose veins in their legs, they can get them in the pelvis too. This can happen after childbirth or because of blood flow being blocked in the veins. The swelling of the veins causes pain sensors in the vein wall to be turned on and cause pain symptoms, and the swollen veins may also press on nerves in the area and cause pain.4
- Gonadal Vein Reflux
The gonadal vein is called the ovarian vein in women and the testicular vein in men. The gonadal vein is different on the right side of the body compared to the left side. On the left side of the body, the gonadal vein starts in the pelvis and connects to the kidney vein. Sometimes blood flows the wrong way in the gonadal vein. One reason for this happening is if there is something blocking the kidney vein, which the left gonadal vein drains into. The blood flowing the wrong way can make the gonadal vein bigger and leads to pain. In women, it can also lead to heavier or more painful periods.4,5
A certain kind of compression of the kidney vein is called nutcracker anatomy. This anatomy can cause pain in your side or blood in your urine, and it is called nutcracker syndrome.
How Can These Problems Be Treated?
Doctors have some ways to help with pelvic vein problems:
- Stents: A small tube can be placed in a squeezed vein to help keep it open so blood flows normally.
- Sclerotherapy or embolization: These are special treatments to close off swollen veins so blood can go through the healthy ones, which can help reduce pain.
All of these treatments are done with small tools through tiny cuts, not big surgeries.6-9


How Is SAFIRE Helping?
Many people with pelvic pain have a hard time getting the right care. Some doctors may not fully understand these vein problems, and some patients feel like their pain is not taken seriously—especially women and men with pelvic pain with no obvious cause.10
SAFIRE is trying to help by:
- Helping researchers learn more about these conditions and possible treatments
- Teaching doctors and patients about these problems
- Raising money for education, resources, and research
If you want to help people with chronic pelvic pain, please visit our donation page to support SAFIRE’s mission.
References
- Ahangari A. Prevalence of chronic pelvic pain among women: an updated review. Pain Physician. 2014;17(2):E141–147.
- Liddell RP, Evans NS. May-Thurner syndrome. Vasc Med. 2018;23(5):493–496.
- Ignacio EA, Dua R, Sarin S, et al. Pelvic congestion syndrome: diagnosis and treatment. Semin Intervent Radiol. 2008;25(4):361–368.
- Corrêa MP, Bianchini L, Saleh JN, Noel RS, Bajerski JC. Pelvic congestion syndrome and embolization of pelvic varicose veins. J Vasc Bras. 2019;18:e20190061.
- Onka B, Khouchoua S, Yehouenou TRT, Jerguigue H, Latib R, Omor Y. Nutcracker syndrome: A rare cause of chronic pelvic pain and left back pain. Radiol Case Rep. 2021;16(8):2025–2030.
- Ahmed O, Ng J, Patel M, et al. Endovascular Stent Placement for May-Thurner Syndrome in the Absence of Acute Deep Vein Thrombosis. J Vasc Interv Radiol. 2016;27(2):167–173.
- Hager ES, Yuo T, Tahara R, et al. Outcomes of endovascular intervention for May-Thurner syndrome. J Vasc Surg Venous Lymphat Disord. 2013;1(3):270–275.
- Lakhanpal G, Kennedy R, Lakhanpal S, Sulakvelidze L, Pappas PJ. Pelvic venous insufficiency secondary to iliac vein stenosis and ovarian vein reflux treated with iliac vein stenting alone. J Vasc Surg Venous Lymphat Disord. 2021;9(5):1193–1198.
- Daniels JP, Champaneria R, Shah L, Gupta JK, Birch J, Moss JG. Effectiveness of Embolization or Sclerotherapy of Pelvic Veins for Reducing Chronic Pelvic Pain: A Systematic Review. J Vasc Interv Radiol. 2016;27(10):1478–1486 e1478.
- McGowan L, Luker K, Creed F, Chew-Graham CA. How do you explain a pain that can’t be seen?: the narratives of women with chronic pelvic pain and their disengagement with the diagnostic cycle. Br J Health Psychol. 2007;12(Pt 2):261–274.
- Meissner MH, Khilnani NM, Labropoulos N, Gasparis AP, Gibson K, Greiner M, Learman LA, Atashroo D, Lurie F, Passman MA, Basile A, Lazarshvilli Z, Lohr J, Kim MD, Nicolini PH, Pabon-Ramos WM, Rosenblatt M. The Symptoms-Varices-Pathophysiology classification of pelvic venous disorders: A report of the American Vein & Lymphatic Society International Working Group on Pelvic Venous Disorders. J Vasc Surg Venous Lymphat Disord. 2021 May;9(3):568-584. doi: 10.1016/j.jvsv.2020.12.084. Epub 2021 Jan 30. PMID: 33529720.
- Liu Y, Zheng H, Wang X, Wang Z, Zhu Q, Wen C, Tong Y. Ultrasound characteristics of abdominal vascular compression syndromes. Front Cardiovasc Med. 2023 Dec 18;10:1282597. doi: 10.3389/fcvm.2023.1282597. PMID: 38173818; PMCID: PMC10764025.
- Bałabuszek, K., Toborek, M., & Pietura, R. (2021). Comprehensive overview of the venous disorder known as pelvic congestion syndrome. Annals of Medicine, 54(1), 22–36. https://doi.org/10.1080/07853890.2021.2014556
Definition and Epidemiology
Chronic pelvic pain (CPP) is defined as non-cyclic pain in the pelvis or lower abdomen persisting for ≥6 months. Global prevalence estimates range from 5.7% to 26.6%, which highlights CPP as a significant yet under-addressed clinical burden.1 Among the numerous etiologies of CPP, a subset stems from pelvic venous disorders (PeVD), which include:
- Iliac vein compression syndrome (e.g., May-Thurner syndrome or non-thrombotic iliac vein lesions [NIVL])
- Pelvic varices
- Gonadal vein reflux
CPP and PeVD often coexist and may contribute to venous hypertension, neuropathic sensitization, and visceral congestion.
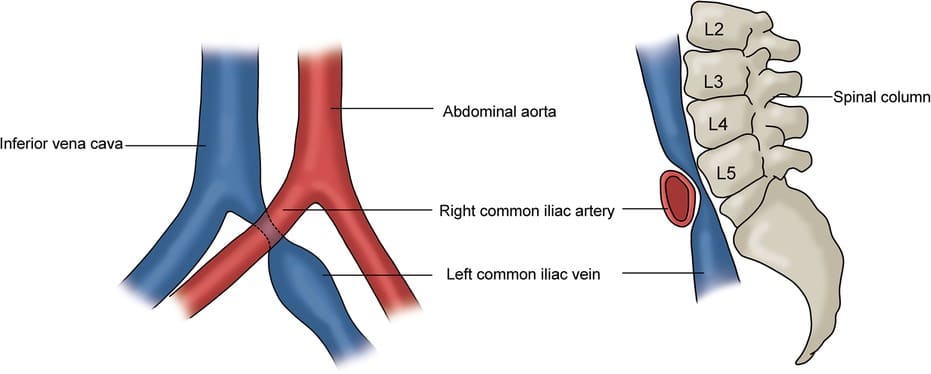
Iliac Vein Compression
Iliac vein compression—most commonly of the left common iliac vein (LCIV) by the overlying right common iliac artery against the vertebral column—is an abundant anatomical variant with numerous potential clinical consequences.2 This extrinsic compression impairs venous outflow from the left lower extremity and pelvis, potentially leading to venous hypertension, reflux, collateralization, and symptomatic venous congestion. A proposed mechanism of action of pelvic venous hypertension causing pain involves direct neurologic effect on the lumbosacral plexus and hypogastric nerve plexuses due to direct compression from engorged collateral draining veins along the neurovascular bundles. This may occur around the pudendal nerve and sciatic nerves lower in the pelvis from obstruction related reflux as well.
Classically, it is taught that iliac vein compression causes left leg pain and swelling, DVT and /or ulceration. Recently, data is emerging to suggest that gastrointestinal symptoms including bloating, constipation, diarrhea (i.e. IBS), urinary symptoms including urinary retention, frequency, urgency and pain (i.e. interstitial cystitis type symptoms), low back pain and SI region/hip pain, dyspareunia, postural orthostatic tachycardia (POTS), upper abdominal pain and nausea and bilateral lower symptoms may actually be more common and unrecognized presentations of iliac vein compression. Cross-sectional imaging (e.g., MRV/CTV), duplex ultrasonography, and intravascular ultrasound (IVUS) are instrumental in diagnosing iliac vein compressions.3 Recent studies have shown the US and CT are inaccurate for diagnosis of iliac vein compression, with MR being much more sensitive and venography with IVUS being the gold standard.
Pelvic Varices
Low deep pelvic varicosities may arise from the internal iliac vein as opposed to the gonadal vein. This occurs either independently or secondary to outflow obstruction or gonadal vein reflux. These dilated venous plexuses cause activation of nociceptors in the vein wall and may compress pelvic nerves and viscera, leading to nociceptive and neuropathic pain.4 Postpartum venous remodeling and pelvic floor trauma further contribute to venous incompetence and pain symptoms. Emerging data would suggest that deep pelvic vein dilation may be related to trauma from vaginal deliveries during birthing. While some patients manifest with visible vulvar varices, many do not. A new technique for US of the perineum has been developed to look for these veins that are best seen by following the rectal signature anteriorly to the posterior wall of the vagina where a cluster of dilated refluxing veins may be present. These veins are not identified on transvaginal US as the probe is inserted to the level of the cervix which is central to the pelvic floor.
Vulvodynia, persistent genital arousal disorder, periurethral pain, rectal tenesmus and pelvic floor pain may be caused by peri clitoral, vaginal wall, perirectal varices which are not visible on colonoscopy or cystoscopy and therefore missed. These veins are very hard to see on MRI or cross-sectional imaging as well.
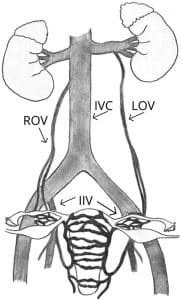
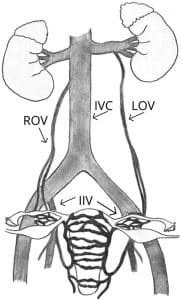
Gonadal Vein Reflux
Gonadal vein reflux refers to retrograde flow within the ovarian (females) or testicular (males) veins. Anatomically, the left gonadal vein drains into the left renal vein, which is susceptible to compression between the aorta and superior mesenteric artery—a configuration referred to as nutcracker anatomy. Classically symptoms were felt to be hematuria and left flank pain, classified as nutcracker syndrome.4
There is an emerging body of data to support that nutcracker contributes to many previously unrecognized symptoms other than flank pain and hematuria. These symptoms may exist in the absence or presence of flank pain. Potential upper abdominal symptoms include gastric dysmotility, post prandial abdominal pain, chest pain, POTS, food fear, nausea, vomiting, back pain and headaches. It is hypothesized that this is related to effects of collateralized venous drainage through the ascending lumbar/ azygous system, diaphragm, transverse lumbar and epidural veins. In women, retrograde flow from the renal vein may lead to pelvic congestion, dysmenorrhea, dyspareunia, and menorrhagia; in men, the analogous condition is a varicocele which can cause testicular/scrotal pain and infertility. Compression of the left renal vein increases the risk of reflux in the left gonadal vein. One mechanism of action of pain elucidation is that reflux activates nociceptors (pressure sensing pain receptors) within the vein wall causing localized pain. There is emerging data to suggest that chronic venous stasis in the pelvis (similar to known and more obvious skin changes for example in the legs) leads to inflammation and toxin build up causing localized inflammation as well. Lower in the pelvis, this can cause engorged veins may interact with surrounding nerves, such as pudendal and sciatic nerves, causing pain.5
Interventions
Iliac Vein Stenting: Endovascular stenting of the LCIV has demonstrated efficacy in alleviating symptoms of pelvic venous outflow obstruction. This minimally invasive intervention restores luminal patency and reduces venous hypertension. Clinical studies have shown significant improvement in patient-reported outcomes after LCIV stenting.6-9

Gonadal Vein Embolization/Sclerotherapy: Embolization (coils, plugs, sclerosants) occludes incompetent pelvic veins, thereby offloading venous hypertension and mitigating nociceptive stimuli from vein wall stretch receptors. Studies have reported symptomatic relief and improved quality of life following these interventions.4,10
These procedures are typically performed percutaneously under fluoroscopic guidance and carry low procedural morbidity when performed by experienced interventionalists.

SAFIRE’s Mission
Despite advancements in diagnostic modalities and interventional treatments, patients with venous etiologies of CPP frequently encounter delays in diagnosis and inadequate or incomplete treatment. One report from McGowan et al. (2007) illustrates the dismissal of patient-reported symptoms, a challenge that often persists today.11 Not only is it difficult for all chronic pelvic pain patients to access effective care options, but there is a lack of research in the CPP and PeVD space.
SAFIRE is committed to addressing this gap through:
- Research funding to elucidate pathophysiology and optimize treatment options
- Education initiatives targeting both patients and healthcare professionals
- Advocacy to ensure equitable and timely access to diagnostic and interventional care
To support SAFIRE’s efforts in transforming care delivery for patients with venous chronic pelvic pain, visit our donation page and consider contributing to our research and education funds.
References
- Ahangari A. Prevalence of chronic pelvic pain among women: an updated review. Pain Physician. 2014;17(2):E141–147.
- Liddell RP, Evans NS. May-Thurner syndrome. Vasc Med. 2018;23(5):493–496.
- Ignacio EA, Dua R, Sarin S, et al. Pelvic congestion syndrome: diagnosis and treatment. Semin Intervent Radiol. 2008;25(4):361–368.
- Corrêa MP, Bianchini L, Saleh JN, Noel RS, Bajerski JC. Pelvic congestion syndrome and embolization of pelvic varicose veins. J Vasc Bras. 2019;18:e20190061.
- Onka B, Khouchoua S, Yehouenou TRT, Jerguigue H, Latib R, Omor Y. Nutcracker syndrome: A rare cause of chronic pelvic pain and left back pain. Radiol Case Rep. 2021;16(8):2025–2030.
- Ahmed O, Ng J, Patel M, et al. Endovascular Stent Placement for May-Thurner Syndrome in the Absence of Acute Deep Vein Thrombosis. J Vasc Interv Radiol. 2016;27(2):167–173.
- Hager ES, Yuo T, Tahara R, et al. Outcomes of endovascular intervention for May-Thurner syndrome. J Vasc Surg Venous Lymphat Disord. 2013;1(3):270–275.
- Lakhanpal G, Kennedy R, Lakhanpal S, Sulakvelidze L, Pappas PJ. Pelvic venous insufficiency secondary to iliac vein stenosis and ovarian vein reflux treated with iliac vein stenting alone. J Vasc Surg Venous Lymphat Disord. 2021;9(5):1193–1198.
- Spencer EB, Schuelke A, Porter K, Nelson J, Horne ES. Improvement of quality of life in women ≤ 25-years-old with chronic pelvic pain following stenting of nonthrombotic iliac vein compression. Phlebology. 2024:2683555241287312.
- Daniels JP, Champaneria R, Shah L, Gupta JK, Birch J, Moss JG. Effectiveness of Embolization or Sclerotherapy of Pelvic Veins for Reducing Chronic Pelvic Pain: A Systematic Review. J Vasc Interv Radiol. 2016;27(10):1478–1486 e1478.
- McGowan L, Luker K, Creed F, Chew-Graham CA. How do you explain a pain that can’t be seen?: the narratives of women with chronic pelvic pain and their disengagement with the diagnostic cycle. Br J Health Psychol. 2007;12(Pt 2):261–274.
- Meissner MH, Khilnani NM, Labropoulos N, Gasparis AP, Gibson K, Greiner M, Learman LA, Atashroo D, Lurie F, Passman MA, Basile A, Lazarshvilli Z, Lohr J, Kim MD, Nicolini PH, Pabon-Ramos WM, Rosenblatt M. The Symptoms-Varices-Pathophysiology classification of pelvic venous disorders: A report of the American Vein & Lymphatic Society International Working Group on Pelvic Venous Disorders. J Vasc Surg Venous Lymphat Disord. 2021 May;9(3):568-584. doi: 10.1016/j.jvsv.2020.12.084. Epub 2021 Jan 30. PMID: 33529720.
- Liu Y, Zheng H, Wang X, Wang Z, Zhu Q, Wen C, Tong Y. Ultrasound characteristics of abdominal vascular compression syndromes. Front Cardiovasc Med. 2023 Dec 18;10:1282597. doi: 10.3389/fcvm.2023.1282597. PMID: 38173818; PMCID: PMC10764025.
- Bałabuszek, K., Toborek, M., & Pietura, R. (2021). Comprehensive overview of the venous disorder known as pelvic congestion syndrome. Annals of Medicine, 54(1), 22–36. https://doi.org/10.1080/07853890.2021.2014556