Ehlers-Danlos Syndromes (EDS) and Hypermobility Spectrum Disorders (HSD)
Ehlers-Danlos syndromes, or EDS, are a group of genetic conditions. This means they are passed down from parents to children through their genes. People with EDS often have very stretchy skin, loose joints, and other body problems.1 There are 14 known types of EDS, and most are caused by changes in certain genes that affect something called collagen, which is a protein that provides structural support for cells and tissues.
- For Patients
- For Physicians
Background
Ehlers-Danlos syndromes, or EDS, are a group of genetic conditions. This means they are passed down from parents to children through their genes. People with EDS often have very stretchy skin, loose joints, and other body problems.1 There are 14 known types of EDS, and most are caused by changes in certain genes that affect something called collagen, which is a protein that provides structural support for cells and tissues.1-3
Doctors can often tell if someone has EDS by their symptoms and by doing a physical exam. Sometimes, they use genetic tests to confirm the diagnosis. One common type of EDS—called hypermobile EDS (or hEDS)—still doesn’t have a known genetic cause, so it can’t be found through a genetic test yet.1
There’s also another group of conditions called Hypermobility Spectrum Disorders, or HSD. People with HSD have very flexible joints and pain, but they don’t meet the full requirements for EDS or hEDS. Doctors will only diagnose someone with HSD after checking to make sure they don’t have one of the types of EDS.4
EDS may affect about 1 in every 5,000 people. The most common type, hEDS, affects around 1 in every 10,000 to 15,000 people.5 Some studies suggest that hEDS and HSD together might affect as many as 1 in 500 people.6
Doctors and scientists are still learning more. EDS and HSD may be linked to other health problems like POTS (a condition that makes your heart race when you stand up), MCAS (which affects allergy-type cells), long COVID, and pelvic venous disorders (PeVD).7-9
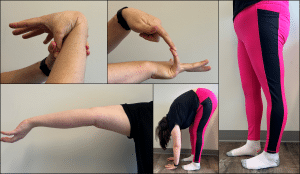
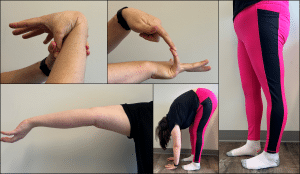
What Are the Symptoms?1,4,10,11
People with EDS or HSD can have different symptoms, depending on the type. Some common signs include:
- Very soft, stretchy skin
- Joints that bend too much or pop out of place
- Bruising easily
- Pain in the joints or pelvis
- Curved spine (scoliosis)
- Problems with healing after cuts
- Bulging veins (varicose veins)
- Stomach issues
- Fatigue
- Weak blood vessels that can break

How Are They Treated?11
There is no cure for EDS or HSD, but there are treatments that can help people feel better and manage their symptoms. These include:
- Medicine for pain control
- Physical therapy
- Making changes in daily habits to avoid injury
- In some cases, surgery (like stabilizing joints), but surgery doesn’t always work well for people with EDS or HSD
If you’re looking for help with EDS or HSD, you can visit SAFIRE’s resources page to find doctors that specialize in EDS.
What Is SAFIRE Doing to Help?
There is a need for better education, more awareness, and further research about EDS and HSD. SAFIRE aims to restore hope in patients by raising funds to support research efforts, to provide resources to patients, and to offer better education for patients and healthcare professionals.
If you are interested in supporting SAFIRE’s mission, please consider contributing through our donation page.
References
- Malfait F, Castori M, Francomano CA, Giunta C, Kosho T, Byers PH. The Ehlers-Danlos syndromes. Nat Rev Dis Primers. 2020;6(1):64.
- Beighton P, de Paepe A, Danks D, et al. International Nosology of Heritable Disorders of Connective Tissue, Berlin, 1986. Am J Med Genet. 1988;29(3):581–594.
- Malfait F, Francomano C, Byers P, et al. The 2017 international classification of the Ehlers-Danlos syndromes. Am J Med Genet C Semin Med Genet. 2017;175(1):8–26.
- Carroll MB. Hypermobility spectrum disorders: A review. Rheumatol Immunol Res. 2023;4(2):60–68.
- Miklovic T, Sieg VC. Ehlers-Danlos Syndrome. In: StatPearls. Treasure Island (FL): StatPearls Publishing
Copyright © 2025, StatPearls Publishing LLC.; 2025. - Demmler JC, Atkinson MD, Reinhold EJ, Choy E, Lyons RA, Brophy ST. Diagnosed prevalence of Ehlers-Danlos syndrome and hypermobility spectrum disorder in Wales, UK: a national electronic cohort study and case-control comparison. BMJ Open. 2019;9(11):e031365.
- Kucharik AH, Chang C. The Relationship Between Hypermobile Ehlers-Danlos Syndrome (hEDS), Postural Orthostatic Tachycardia Syndrome (POTS), and Mast Cell Activation Syndrome (MCAS). Clin Rev Allergy Immunol. 2020;58(3):273–297.
- Pollack B, von Saltza E, McCorkell L, et al. Female reproductive health impacts of Long COVID and associated illnesses including ME/CFS, POTS, and connective tissue disorders: a literature review. Front Rehabil Sci. 2023;4:1122673.
- Ormiston CK, Padilla E, Van DT, et al. May-Thurner syndrome in patients with postural orthostatic tachycardia syndrome and Ehlers-Danlos syndrome: a case series. Eur Heart J Case Rep. 2022;6(4):ytac161.
- Parapia LA, Jackson C. Ehlers-Danlos syndrome–a historical review. Br J Haematol. 2008;141(1):32–35.
- Castori M. Ehlers-danlos syndrome, hypermobility type: an underdiagnosed hereditary connective tissue disorder with mucocutaneous, articular, and systemic manifestations. ISRN Dermatol. 2012;2012:751768.
- Lindholm, S., Petersson, S., Molander, P. and Björk, M. (2025), The Impact of Pain on Everyday Activities of People With Hypermobility Spectrum Disorders or Hypermobility Ehlers Danlos Syndrome. Eur J Pain, 29: e70000.
Background
Ehlers-Danlos syndromes (EDS) are a clinically and genetically heterogeneous group of connective tissue disorders characterized by joint hypermobility, skin hyperextensibility, and tissue fragility.1 The 2017 international classification delineates 13 clinically distinct EDS subtypes; each associated with mutations in one of 19 genes, most of which encode proteins involved in the biosynthesis or structure of collagen or related extracellular matrix components.2,3 Since the 2017 classification, researchers have identified one additional type of EDS caused by one associated genetic mutation.1 This brings the total number of EDS types to 14 caused by changes in one of 20 genes. Mutations affecting collagen fibrillogenesis, cross-linking, or structural integrity account for the classical features observed in many EDS patients.
A subset of patients present with EDS-like phenotypes but test negative for known pathogenic variants. This suggests that additional, unidentified genetic variants or subtypes may exist.1 Clinical diagnosis remains essential, especially in subtypes lacking definitive molecular markers.
Of particular relevance is hypermobile EDS (hEDS), the most prevalent subtype. The underlying genetic etiology remains unknown for hEDS, complicating genetic confirmation. Consequently, hEDS remains a diagnosis of exclusion based on strict clinical criteria.1
Hypermobility spectrum disorders (HSD) represent a broader group of conditions encompassing symptomatic joint hypermobility in individuals who do not meet the diagnostic criteria for hEDS or other defined EDS subtypes.4 The diagnostic process requires a comprehensive evaluation to exclude other forms of EDS and typically involves multiple clinical assessments by experienced clinicians.4
Prevalence
Epidemiologic data estimates the prevalence of all EDS types at approximately 1 in 5,000 individuals, though subtype-specific prevalence is poorly defined. hEDS alone is estimated to occur in 1 in 10,000 to 15,000 individuals.5 A population-based study in Wales suggested a combined prevalence of hEDS and HSD of approximately 1 in 500 individuals, indicating under-recognition and likely diagnostic delays.6
Recent literature has explored potential comorbidities and associations with EDS/HSD, including postural orthostatic tachycardia syndrome (POTS), mast cell activation syndrome (MCAS), long COVID, and iliac vein compression syndrome (May-Thurner syndrome), though mechanistic links remain under investigation.7-9
Clinical Presentation1,4,10,11
The clinical phenotype varies by subtype and individual but frequently includes:
- Generalized joint hypermobility
- Recurrent joint subluxations or dislocations
- Chronic musculoskeletal pain
- Skin hyperextensibility and fragility
- Abnormal wound healing
- Easy bruising
- Pelvic pain
- Spinal pain or scoliosis
- Vascular fragility (in vascular EDS)
- Gastrointestinal dysmotility or functional symptoms
- Fatigue and autonomic dysfunction

Management Strategies
Currently, there is no curative treatment for EDS or HSD. Management focuses on symptom control, functional improvement, and prevention of complications. Multimodal pain management strategies—including pharmacologic agents, physical therapy, and tailored lifestyle modifications—form the cornerstone of care. Orthopedic or neurosurgical interventions such as joint stabilization or tendon relocation may be considered in refractory cases but are associated with variable outcomes and higher failure rates due to underlying tissue fragility.11
Effective long-term management typically requires a multidisciplinary approach involving physical medicine, pain specialists, rheumatologists, geneticists, and when necessary, surgical consultation.
The link between venous stasis and hypermobility is in the early stages of study but in a study of women with POTS and pelvic pain 38% of patients reported hypermobility, and there may be an increased risk of vascular complications of long COVID and compression syndromes in patients with connective tissue defects.
Providers seeking expert consultation and patients looking for specialized care may refer to SAFIRE’s curated list of experienced providers and resources.
SAFIRE’s Role
Given the challenges in diagnosis and treatment and the under recognition of EDS and HSD, SAFIRE is focused on increasing clinician and public awareness, supporting clinical and genetic research, and providing educational resources to patients and healthcare professionals. SAFIRE aims to improve diagnostic accuracy, enhance access to multidisciplinary care, and ultimately improve quality of life for affected individuals in regard to the interaction of hypermobility and venous disease.
Patients, physicians, and researchers interested in supporting SAFIRE’s mission may contribute through our donation page.
References
- Malfait F, Castori M, Francomano CA, Giunta C, Kosho T, Byers PH. The Ehlers-Danlos syndromes. Nat Rev Dis Primers. 2020;6(1):64.
- Beighton P, de Paepe A, Danks D, et al. International Nosology of Heritable Disorders of Connective Tissue, Berlin, 1986. Am J Med Genet. 1988;29(3):581–594.
- Malfait F, Francomano C, Byers P, et al. The 2017 international classification of the Ehlers-Danlos syndromes. Am J Med Genet C Semin Med Genet. 2017;175(1):8–26.
- Carroll MB. Hypermobility spectrum disorders: A review. Rheumatol Immunol Res. 2023;4(2):60–68.
- Miklovic T, Sieg VC. Ehlers-Danlos Syndrome. In: StatPearls. Treasure Island (FL): StatPearls Publishing
Copyright © 2025, StatPearls Publishing LLC.; 2025. - Demmler JC, Atkinson MD, Reinhold EJ, Choy E, Lyons RA, Brophy ST. Diagnosed prevalence of Ehlers-Danlos syndrome and hypermobility spectrum disorder in Wales, UK: a national electronic cohort study and case-control comparison. BMJ Open. 2019;9(11):e031365.
- Kucharik AH, Chang C. The Relationship Between Hypermobile Ehlers-Danlos Syndrome (hEDS), Postural Orthostatic Tachycardia Syndrome (POTS), and Mast Cell Activation Syndrome (MCAS). Clin Rev Allergy Immunol. 2020;58(3):273–297.
- Pollack B, von Saltza E, McCorkell L, et al. Female reproductive health impacts of Long COVID and associated illnesses including ME/CFS, POTS, and connective tissue disorders: a literature review. Front Rehabil Sci. 2023;4:1122673.
- Ormiston CK, Padilla E, Van DT, et al. May-Thurner syndrome in patients with postural orthostatic tachycardia syndrome and Ehlers-Danlos syndrome: a case series. Eur Heart J Case Rep. 2022;6(4):ytac161.
- Parapia LA, Jackson C. Ehlers-Danlos syndrome–a historical review. Br J Haematol. 2008;141(1):32–35.
- Castori M. Ehlers-danlos syndrome, hypermobility type: an underdiagnosed hereditary connective tissue disorder with mucocutaneous, articular, and systemic manifestations. ISRN Dermatol. 2012;2012:751768.
- Lindholm, S., Petersson, S., Molander, P. and Björk, M. (2025), The Impact of Pain on Everyday Activities of People With Hypermobility Spectrum Disorders or Hypermobility Ehlers Danlos Syndrome. Eur J Pain, 29: e70000.