Postural Orthostatic Tachycardia Syndrome
Postural Orthostatic Tachycardia Syndrome (POTS) presents a significant challenge in the realm of healthcare, often acting as a hidden cause behind chronic symptoms such as dizziness, fatigue, and heart palpitations. Unfortunately, it is frequently misdiagnosed or overlooked, leaving patients navigating a frustrating journey through multiple doctors, years of unrelenting symptoms, and a variety of treatments that may offer minimal relief.
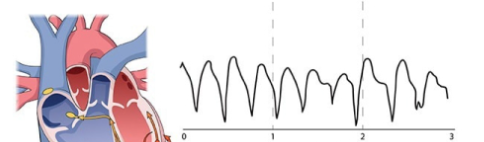
The range of symptoms associated with POTS primarily stems from dysregulation of the autonomic nervous system, which controls critical functions like heart rate, blood pressure, and blood flow. When standing, the body fails to adjust properly, resulting in a rapid heart rate, dizziness, fatigue, and other distressing symptoms. Without proper management, these symptoms often intensify, significantly impacting a patient’s ability to function on a daily basis. Complicating the situation further, many patients with POTS have other overlapping conditions, such as Ehlers-Danlos syndrome, mast cell activation syndrome, or chronic fatigue syndrome, making both diagnosis and treatment more complex.
In recent years, however, growing evidence has shed light on a potentially overlooked contributor to POTS symptoms: pelvic venous congestion and chronic venous insufficiency, particularly involving the iliac veins. In some patients, the iliac veins—the large veins in the pelvis that drain blood from the legs—become compressed or obstructed, leading to poor venous return, blood pooling, and increased pressure in the lower extremities. This condition, often referred to as iliac vein compression syndrome or May-Thurner syndrome, can exacerbate POTS symptoms, particularly when combined with the autonomic dysfunction characteristic of POTS.
For many patients, the use of iliac vein stenting, a minimally invasive procedure that opens up blocked or compressed veins, has shown promising results in reducing symptoms of both venous insufficiency and POTS. By improving venous return and blood circulation, iliac vein stenting may help alleviate some of the circulatory issues that contribute to the rapid heart rate, dizziness, and fatigue that POTS patients experience.
These coexisting conditions—venous insufficiency and autonomic dysfunction—can worsen POTS symptoms and require an even more nuanced approach to care, highlighting the importance of a comprehensive understanding of each patient’s medical history and underlying health factors. The presence of hypermobile joints, mast cell activation, and other related disorders can cause a cascade of additional challenges, from more severe dizziness and pain to greater difficulty managing stress and physical activity.
Despite the disabling effects of POTS on patients’ lives, treatment approaches often face significant barriers, including limited insurance coverage and inconsistent recognition of the condition within the medical community. Many POTS patients struggle to access the specialized care they need, as the condition is not always well understood, and medical practitioners may be hesitant to prescribe treatments that are seen as experimental or outside standard protocols.
Recent studies have brought attention to important insights into the condition, including the role of blood volume, vascular health, and autonomic regulation. It has become increasingly clear that iliac vein stenting—can have a meaningful impact on symptom relief. However, more research is needed to uncover the full spectrum of underlying mechanisms and to refine treatments that can effectively improve quality of life for POTS sufferers.
Given these complexities, there is an urgent need for greater recognition, insurance reform, and dedicated research efforts aimed at understanding POTS more thoroughly. Through enhanced awareness, evidence-based approaches, and more accessible treatment options like iliac vein stenting, we can better support individuals living with POTS, providing them with the tools and interventions necessary to regain control of their health and well-being.